How Does HIV cause AIDS?
AIDS (acquired immunodeficiency syndrome) is a devastating disease, caused by infection of HIV (human immunodeficiency virus). There were around 39 million people infected with HIV in 2022 . But not everyone who is infected with HIV gets AIDS. In fact, with proper treatment, most people who are HIV-infected go on to live long and healthy lives.
However, people who are not treated effectively may develop AIDS over a period of time. AIDS is a deleterious condition, with over 630,000 people dying from AIDS-related illnesses worldwide in 2022.
For World AIDS Day this, the theme is ‘remember and commit.’ In order to commemorate those who have lost their lives to this deleterious disease, we dedicate this piece to understanding how the virus works and its impact on the body’s immune system.
To fully understand the effects of the disease and for the development of suitable therapeutics, it’s important to understand the biology of HIV infection and how it can cause AIDS.
This article will explain the life cycle of HIV and the development of AIDS.
Biology of the HIV life cycle
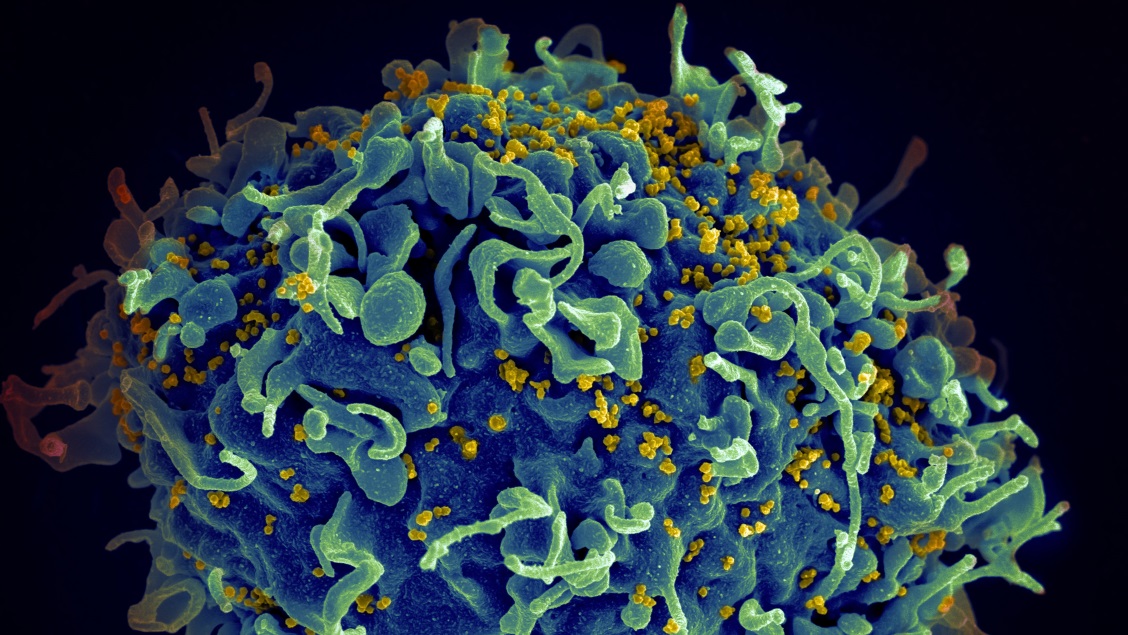
HIV targets specific immune cells in the body called helper T cells. HIV uses these cells to replicate. Once the virus successfully replicates, it goes on to infect other helper T cells. This cycle of infection and replication is complex and comprises multiple steps.
We will go through the stages of HIV infection, and explain what happens at each step.
Receptor binding and fusion
On the surface of HIV, there are specific proteins called envelope proteins. These proteins are complementary to receptor proteins on helper T cells, called CD4. This means they are able to bind together, like a lock and key. When the envelope and CD4 proteins bind together, it enables fusion with the helper T cell. From here, the virus cells use the helper T cell as its host cell for replication.
Transfer of genetic material
The genetic material of HIV is known as RNA. RNA holds all the essential viral information, possessing unique codes to make every single protein of the virus. The RNA of HIV is held in a protective coating, called the capsid.
Once the virus has fused with the helper T cell, the capsid is ‘injected ’ into the cell. After entering the cell, the RNA within the capsid starts to multiply.
Integration of RNA into host DNA
Every single cell in the human body contains genetic information, called DNA. Similar to RNA, the host DNA is responsible for all cell functions and the production of proteins.
HIV is a type of virus called a Retrovirus, which means it fuses its own RNA with the host’s DNA. To do this, the capsid (which contains the RNA) is transported by helpful motor proteins that ‘walk’ the capsid along fibres in the cell. These fibres function as a network of roads in the cell.
The capsid is guided to the nucleus of the cell, which contains the host cell’s DNA. Additional proteins help the viral capsid enter the nucleus. Once it enters, the RNA is released from the capsid completely. It is here where the RNA is able to integrate with the host cell DNA.
Viral RNA integration is an intelligent and intricate mechanism that viruses have developed to ‘hijack’ the host cell’s machinery. This means that, after integration, the host cell uses the viral RNA code to produce viral proteins like it would its own proteins.
Building a new virus
The HIV virus is made up of 1) proteins and 2) RNA. The production of proteins from the genetic code is called ‘translation’.
For the virus to replicate, it uses the cell’s machinery to produce new proteins and replicate its RNA. The cell uses the integrated viral RNA as a code.
The initial steps of protein production occur within the nucleus and end just outside the nucleus.
Once the proteins are produced and the RNA is replicated, they are transported to the surface of the host cell. Here, the new virus is assembled.
A series of complex steps result in the new virus budding off the surface of the cell. This leaves the virus free to spread throughout the body, infecting other helper T cells.
Latency stage
Translation of viral proteins doesn’t always happen straight away. In some cases, there is a stage in which the virus lies dormant. This means that the viral RNA stays integrated within the host cell’s DNA but does not get translated into proteins. This stage is called the latency stage, and it can last anywhere from a few days to years, or even a lifetime.
This dormancy means the virus is able to ‘hide’ in host cells and does not produce more virus. Therefore, the immune system cannot detect infected cells. Many infected people at this stage do not even know they are infected with HIV if they do not test themselves, despite living with the virus for years.
With HIV lying dormant in host cells, a reservoir of latent viruses are created, which poses a major hurdle for researchers. This is because there is no way to recognise which cells are infected to clear the virus, due to the virus’s excellent ability to remain undetected.
After initial HIV infection, most patients experience a period of acute infection. This means there is a high rate of viral replication and spread of the virus in the body. After this, the period of latency ensues, until activation of the virus occurs again.
How does HIV cause AIDS?
As discussed, HIV is a type of virus that infects helper T cells in our body. These T cells are instrumental in protecting our bodies against pathogens and producing an immune response.
Why do HIV-infected helper T cells die?
During the acute phase of infection, levels of helper T cells rapidly deteriorate. This is because, after infection, the cells recognise a foreign presence in the cell and trigger a complex signalling pathway called apoptosis. This is the process of cell death. Hence, when HIV is active, it causes the death of infected cells.
The importance of helper T cells
Helper T cells are instrumental in overcoming infection. As their name suggests, the T cells help to recruit other immune cells. These immune cells play an important role in directly recognising and killing pathogens. This includes cells that produce antibodies. Antibodies are vital proteins released from immune cells that remove unwanted substances from the body.
What happens when too many helper T cells die?
When helper T cells reach a critically low level, the body is extremely vulnerable to infection from other pathogens.
The normal level of helper T cells in a healthy individual is around 500-1500 cells/mm3. HIV-infected individuals are diagnosed with AIDS when the level of T cells drops to around 200 cells/cm3.
At this point, the body has a significantly weakened immune system. This can result in the development of serious diseases including pneumonia, tuberculosis, meningitis and even some types of cancers. These are termed AIDS-related diseases.
Oftentimes, the body can become too overwhelmed and can no longer cope. With the body acquiring multiple infections or diseases, this can result in the death of the individual.
This is where we recognise the need for treatment and the urgent requirement of a vaccine.
Future work
Since the HIV/AIDS epidemic in 1981, researchers have been trying to understand the complex virus and its interactions with the host. This is so we can work towards the development of suitable therapeutics.
Need for a vaccine
There is currently no approved vaccine and therefore no protection against the virus. Clinical trials have been carried out over the past 10 years, and continue to do so. However, the complex nature of the virus, and its ability to form latent reservoirs, makes it immensely difficult to develop a suitable vaccine.
The triumph of the SARS-CoV-19 RNA vaccine in 2020, has inspired and led to the use of this ground-breaking mRNA technology for development of a HIV vaccine.
The mRNA vaccines for HIV is currently under phase one clinical trials, where three different vaccines are being tested on patients. The study, called HVTN 302, will evaluate the safety of the vaccines and the immune responses of the uninfected patient.
In theory, each of these vaccines will result in the production of proteins found on the surface of HIV. As a result, an immune response should be induced. When the patient is infected with HIV, the patient would then be able to amount an immune response to the virus and clear infection quickly.
We look forward to seeing the outcomes of this exciting and promising clinical trial.
Targeting HIV latent reservoirs
The concept of . This article points out that despite the virus not being actively replicated in helper T cells during latency, there are still other molecular and cellular processes taking place. These processes could play a role in the maintenance of the reservoirs.
Developing therapeutics that could target components in these pathways could be a potential way to clear viral reservoirs and even work towards a cure.
Currently approved medication for HIV, called anti-retroviral therapy, prevents the virus from replicating but does not eradicate the virus or clear viral reservoirs.
A call for research on HIV/AIDS
In light of World AIDS Day, we recognise the importance and need for more research on HIV. This includes a broader understanding of the virus and the development of suitable therapeutics.
MDPI’s Viruses and Vaccines have a selection of research on HIV and AIDS. This research is submitted by researchers aiming to comprehend the impact the virus has on both a biological and psychological level.
If you would like to submit your research, check out MDPI’s full list of journals










Wonderful informations