Rehabilitation in Children with Acute Flaccid Myelitis (AFM)
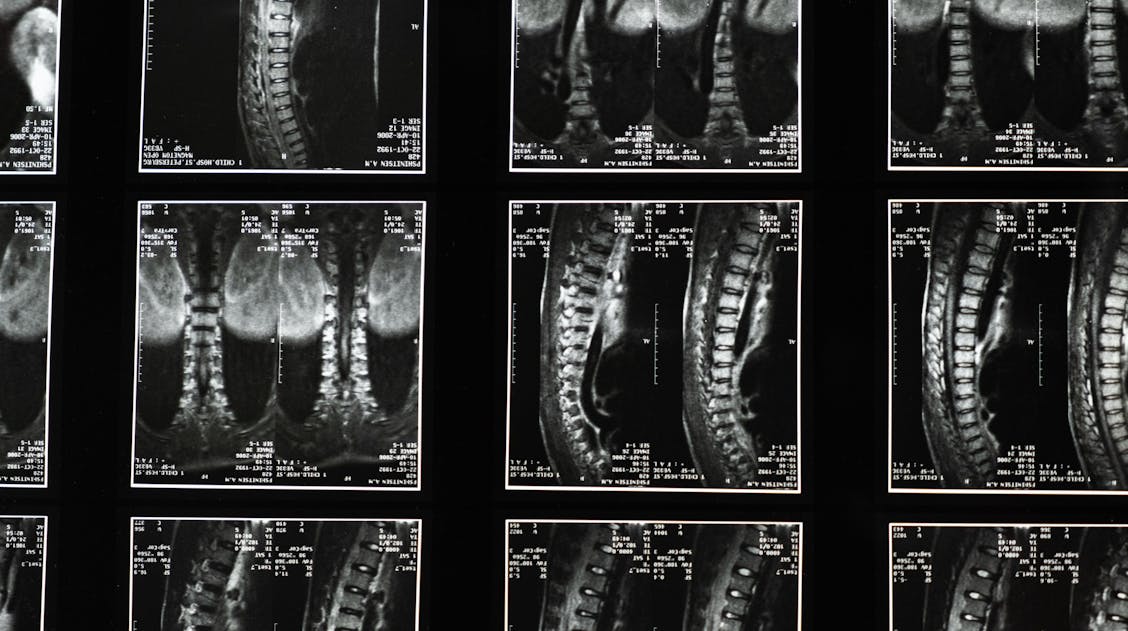
Acute flaccid myelitis (AFM) is a rare but serious neurological condition found predominantly in children. The direct cause of the condition is not fully understood; however, its onset has been linked to infection by enteroviruses. This is a known, rare complication of enteroviruses. The virus attacks the spinal cord, resulting in inflammation, primarily affecting the ventral cord and the anterior horn cells in the grey matter, causing rapid onset of paralysis. In the Open Access journal Children, researchers recently investigated the use of transcutaneous spinal stimulation (TSS) to improve walking outcomes in children diagnosed with AFM.
Acute flaccid myelitis treatment
The prognosis of this condition varies. Research shows that 41% of children affected show full recovery or minimal neurological deficits after 1 year. However, many children often have lasting effects, including residual arm paralysis (75%), residual leg paralysis (60%), deficits in walking ability (58%), and persistent fatigue. These impairments can greatly impact the children’s lives and their independence.
AFM rehabilitation differs from other conditions due to it predominately affecting children. Unlike adults, children need unique rehabilitation through therapy, which guides children through their developmental patterns. This often includes introducing skills that haven’t yet been learnt. As well as keeping growth and maturation in mind rather than restoring functions as in adult rehabilitation. There are currently no guidelines specific to ATM concerning recovery-centred interventions.
Transcutaneous spinal stimulation and Acute flaccid myelitis
TSS is a non-invasive therapy where electrodes stimulate spinal circuitries and initiate a motor response. Moreover, the electrodes are placed on the skin, and the electrical current travels from the skin to the spine. The electrical current amplifies the volume of signals transmitted from the brain to the spinal cord.
Researchers have found that TSS can improve mobility of certain limbs and muscles in children; this includes trunk control, sitting posture, and hand function. There are concerns about using TSS therapy on children, including whether children can tolerate stimulation from the electrodes. In adults, TSS in combination with body-weight supported treadmill training (BWSTT) has been reported to improve postural control, gait mechanics, and motor outputs in adults with spinal cord injuries. However, this combination has not yet been tested on paediatric AFM patients.
In particular, current research focuses on the pharmaceutical treatment and surgical intervention of AFM during acute diagnosis. Because of this, researchers from the International Center for Spinal Cord Injury, Hugo W. Moser Research Institute at Kennedy Krieger Institute and Johns Hopkins University designed a therapy course over 5-8 weeks for children diagnosed with incomplete spinal cord injury secondary to AFM. The course included combining BWSTT and TSS and analysing the participants for any changes in walking function.
Analysis of the TSS and BWSTT
Four outpatient participants were recruited from the International Centre for Spinal Cord Injury at Kennedy Krieger Institute. The participants all had to qualify for the study using the following criteria:
- Within the age range of 6-16 years
- >6 months since the onset of their SCI.
- The SCI had to be non-progressive.
- Neurological injury level above T10
- Tolerates the upright position for >30 mins
- Able to advance one lower extremity in standing without physical assistance
- Be medically stable
- Able to comply with International Standards for Neurological Classification in Spinal Cord Injury
The participants completed 22 rounds of 2-hour therapy sessions 3-5 times per week over 5-8 weeks. These sessions consisted of TSS paired with BWSTT for the first 30 minutes of each session. This was followed by 90 minutes of further training without stimulation. The researchers assessed walking function using four different tests. This included the 6-minute walk test (6MWT), the 10-meter walk test (10MWT), the timed up-and-go test (TUG), and the walking index for spinal cord injury II (WISCI-II). These assessments measured multiple dimensions of gait, including speed and endurance.
Assessing walking function
The 6MWT measured how far a participant walked in six minutes, used to assess walking ability. Furthermore, the 10MWT measured the period it took for a participant to walk 10 meters; it’s used to access neurological movement. The TUG test measured how quickly a participant can stand up from a chair and walk to a marked line and back to the chair, this is to analysed balance and mobility. Finally, the WISCI-II test is used to assess how much physical assistance is needed and what devices are needed to support walking following paralysis from SCI.
Assessing Neurological Change
The International Standards for Neurological Classification in Spinal Cord Injury (ISNCSCI) was used to assess neurological change. This is a 36-item short-form survey (SF-36) that is used to gain background information on the participant’s overall health, participation, and quality of life. The survey was administered at pre- and post-assessment sessions.
Future AFM rehabilitation for children
This study was unique to other research studies in this field because it tested the use of TSS in combination with BWSTT for children diagnosed with AFM. It addressed one of the main concerns around TSS and children: the tolerability of stimulation. All participants of the study reported having hypersensitivity in their trunk and lower extremities during the ISNCSCI survey before the assesement sessions. Despite this, the researchers reported that the participants tolerated the stimulation parameters well and had no reports of pain.
The simulation used in the study did not involve carrier frequency, which the researchers suggest improves tolerability. Additionally, the researchers found that three out of four of the participants experienced greater endurance and activity tolerance in the 6MWT following TSS and BWSTT therapy. These changes exceeded the minimal clinically important difference (MCID), proving the significance of this therapy.
“It’s encouraging to witness the transformations in these children; TSS is revolutionising the field of neurorehabilitation, providing a safe alternative to the aggressive surgeries often required for young patients.” Dr. Rebecca Martin, author on paper.
The researchers demonstrate the safety of TSS in combination with BWSTT for children diagnosed with AFM. Additionally, the researchers identified that the TSS and BWSTT treatments in children may supplement gait-based interventions and facilitate improvements in walking function.
“This treatment is giving families a long-awaited solution when they previously had no answers,” said Martin. Now our goal is to continue refining this approach and make it more widely available to these rare patients across the country”. – Dr. Rebecca Martin.
If you would like to read more or submit research on this topic, please see the Special Issue: Emerging Trends in Neuromodulation for Children with Neurological Conditions.