Tracking Antimicrobial Resistance Using New Methods.
Antimicrobial resistance (AMR) is a serious risk to animal, human and environmental health.
According to the World Health Organization , AMR “is one of the top global public health and development threats. It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.”
AMR is driven by the common misuse and overuse of antibiotics in humans, animals and plants. Because of this, antibiotics are more abundantly distributed in wastewater, allowing more opportunities for bacteria to develop and exchange resistance genes against them.
It’s important to track where and how many of these resistant bacterial colonies exist, but traditional monitoring methods require rigorous preparation and cultivation of these colonies. These methods often require high-cost laboratory systems and take time to produce results.
Because of this, researchers from the US tested the novel integration of a handheld sequencing device in a pilot study published in the Open Access journal Antibiotics to track Escherichia coli (E. coli) and drug-resistant E. coli, also known as extended-spectrum beta-lactamase (ESBL) E. coli, a key indicator of antimicrobial resistance.
Importance of tracking antimicrobial resistance
Antibiotics were first discovered in 1928 when Dr Alexander Fleming observed that a mould, from which later penicillin was later isolated, inhibited the growth of Staphylococcus aureus on an open petri dish in his laboratory, noting that the Staphylococcus strain avoided growing around the mould.
Since this groundbreaking discovery, many variations of antibiotics have been identified and primarily used to treat bacterial infections. However, they have also proven useful in other industries, including agriculture, livestock farming, fermentation and wastewater treatment. As the uses of antibiotics diversify, so does the opportunity for increased AMR.
Antibiotics are lifelines for the treatment of serious bacterial infections such as sepsis. However, AMR develops from the overuse and overproduction of antibiotics. This results in the prolonged exposure of bacteria to antibiotics, allowing the bacteria to evolve and evade the effects of antibiotics.
There are various mechanisms in which bacteria can become resistant to antibiotics, including intrinsic resistance, acquired resistance, genetic change and DNA transfer. All of these mechanisms prevent antibiotics from treating bacterial infections, which can result in the development of superbugs, which are difficult to treat.
The Global Research on AntiMicrobial Resistance Project (GRAM) predicts that bacterial antimicrobial resistance (AMR) will cause 39 million deaths between 2025 and 2050 – equating to three deaths every minute. Because of this, it’s crucial that we find new, quick and effective methods to track these resistant strains of bacteria.
The project is rooted in the One Health Framework, which recognises that human, animal and environmental health are deeply interconnected.
The researchers evaluated the costs and benefits of integrating the handheld nanopore MinION system for E. coli into a culture-based slaughterhouse–river surveillance system.
When explaining their choice of resistant pathogen “It’s not the nastiest one, but it is on the CDC list of pathogens of concern,”- explained Dr Voth-Gaeddert, author on the study.
He further explained “We often use it as a primary indicator of antibiotic resistance.“
Antimicrobial resistance spreading via slaughterhouses
Antibiotics are commonly used to treat infections in animals and to promote animal growth in food-producing animals. Because of this, it’s common for resistant bacteria to colonise in animals’ digestive systems. These bacteria can contaminate meat and the wastewater produced during the slaughter process, which is often released into nearby rivers.
Using new methods to track drug-resistant E.coli
The researchers collected water samples from six chicken slaughterhouses, pre- and post-treatment effluent, as well as upstream and downstream samples from surrounding rivers. All samples were collected during operational hours and more than 12 hours after any significant rain event.
The researchers collected 1000 mL from each sample point. The samples were then immediately homogenised via light physical shaking for 30 seconds. The sample was then split into a 600 mL bottle and a 250 mL bottle for direct DNA extraction for metagenomic sequencing and the Tricycle Protocol, respectively.
Comparing new methods against traditional laboratory techniques
The Tricycle Protocol was first developed by the WHO in 2017. It focuses on the surveillance of ESBL E. coli strains. In the study, the researchers serially diluted the samples, then filtered them using a sterile filter.
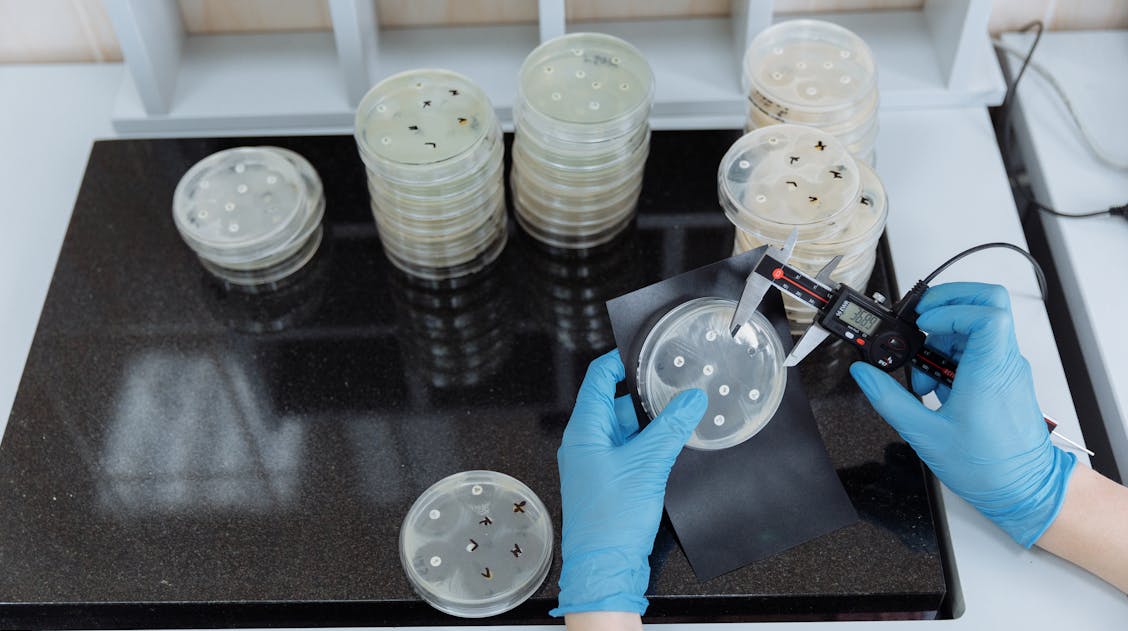
This was then placed onto selective agar used to cultivate drug-resistant E. coli strains and incubated at 37°C for 24 hours. Following the incubation, the researchers counted the colonies on the plates. They then transferred those with the most colonies to fresh agar plates to incubate for further analysis.
The researchers then further analysed the samples to confirm the presence of E. coli using a range of microbiology analysis techniques, including the Sulphide Indole Motility (SIM) test, methyl red and Voges–Proskauer (MRVP) tests, and citrate tests.Finally, the researchers used the double-disc method to confirm the drug-resistant E. coli colonies.
The double disc method is used to detect resistance mechanisms in samples by examining the interactions between two different antibiotics against microbes. The sample is spread onto the agar plate, and antibiotic discs are placed in the middle to see if the antibiotic inhibits bacterial growth, producing a notable ring around the antibiotic.
The researchers also conducted antimicrobial susceptibility testing (AST) using disc diffusion methods; they tested the effectiveness of 14different antibiotics against the sample.
Moreover, the researchers also used benchtop DNA sequencing analysis using the Illumina MiSeq and compared the results against the portable Oxford Nanopore MinION system.
Using portable DNA sequencing for tracking resistant strains
The researchers identified that there were higher concentrations of E. coli and a higher abundance and diversity of antimicrobial-resistant genes in the effluent samples in comparison to river water samples.
They also successfully demonstrated that the portable Oxford Nanopore MinION system produced similar outputs to both the benchtop sequencing system and the antimicrobial susceptibility testing (AST).
“If we only use a narrow lens, we miss a lot of potential leverage points to control the spread of antibiotic resistance,” Dr.Voth-Gaeddert explains. “There’s a lot of opportunity here. That’s why there’s been such a big push to promote One Health.”
The use of fast, affordable and accessible tools such as the Oxford Nanopore MinION system has the power to grow our capabilities of tracking antimicrobial resistance strains. Helping to further the One Health Approach in preventing, predicting and detecting possible health threats.
If you enjoyed this article and would like to read more or submit research about microbiological surveillance, please see the Special Issue: Microbial Resistance Surveillance and Management in Food Systems