Youth-Onset Diabetes And Neurodegenerative Disease Risks
While adult-onset diabetes is known to raise the risk of neurodegenerative diseases, its effect on younger individuals remains underexplored.
In a study published in the open access journal Endocrines, researchers from the University of Colorado at Anschutz indicate that youth-onset diabetes may increase the risk of Alzheimer’s disease and other related neurodegenerative diseases.
In this proof-of-concept study, the researchers detail the presence of specific blood biomarkers that indicate early signs of neurodegeneration and Alzheimer’s disease in young individuals with diabetes. This includes both type 1 and type 2 diabetes.
Alzheimer’s disease is commonly perceived as a late-life condition. The study adds to the underexplored area of its effect on younger individuals by highlighting the potential influence of early-life factors on its development. This article explores the authors’ preliminary evidence suggesting the presence of preclinical Alzheimer’s disease neuropathology in individuals with youth-onset diabetes, indicating a heightened risk of neurodegenerative diseases.
Diabetes and neurodegenerative disease
Diabetes, a chronic condition arising from insufficient insulin production or ineffective insulin utilisation by the body, is associated with an increased risk of neurodegenerative diseases, such as Alzheimer’s disease, particularly diagnosed in older adults.
Most research investigating the link between Alzheimer’s disease and diabetes has traditionally centred around individuals over the age of 40. Within this age group, patients diagnosed with diabetes have a 60 to 80% higher likelihood of developing dementia and potentially Alzheimer’s disease, compared to healthy adults over the age of 40.
What makes Alzheimer’s disease particularly challenging is that its neuropathology begins to develop decades before symptoms appear. In early years, individuals with youth-onset diabetes may experience an increased risk of neurodegenerative disease due to factors such as hyperglycemia and insulin resistance, which are fundamental to the pathophysiology of diabetes.
Biomarkers of neurodegeneration in young individuals
The researchers conducted the study by assessing patient data from three groups of young individuals. One group with type 1 diabetes, one with type 2 diabetes, and a control group without diabetes.
The team aimed to bridge the gap in the literature by investigating the potential link between youth-onset diabetes, neurodegeneration, and Alzheimer’s disease. The researchers focused on the following four key components: comparing plasma biomarkers, tracking changes in these biomarkers, exploring the relationship between the biomarkers and cognitive functions, and addressing differences in clinical imaging biomarkers.
First, they compared plasma biomarkers of Alzheimer’s disease between individuals with youth-onset diabetes and age-matched controls. Secondly, they aimed to track changes in these biomarkers over time among patients with diabetes. Next, they assessed the relationship between biomarker changes and cognitive function in young adulthood. Lastly, the team sought to address differences in the gold-standard clinical imaging biomarkers of Alzheimer’s disease neuropathology between the patient groups.
Initially, the researchers focused on blood biomarkers and PET scans to search for evidence of neurodegenerative disease in young adults with diabetes.
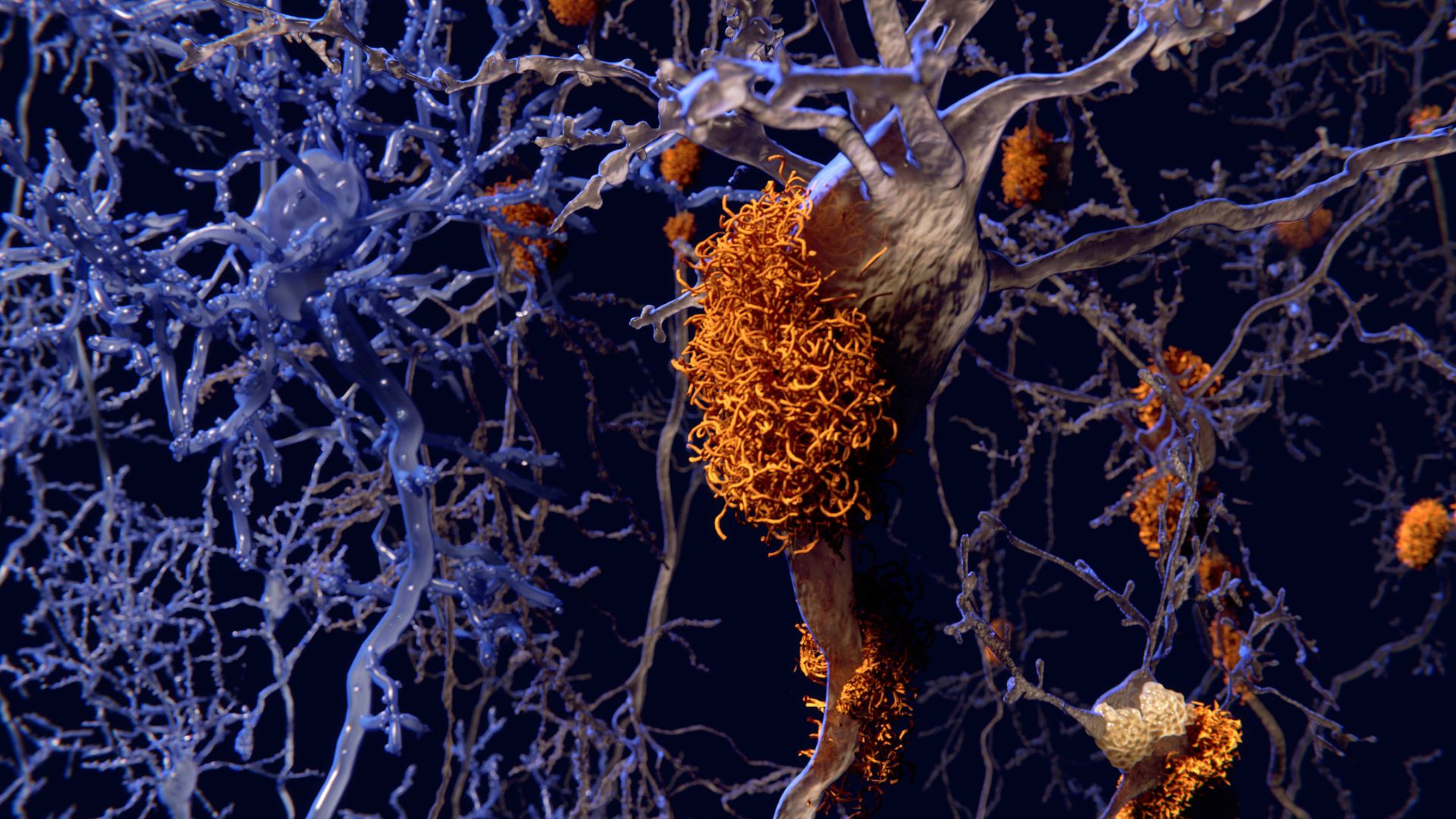
The research team found that alongside the heightened blood biomarkers for Alzheimer’s disease observed in individuals with youth-onset diabetes, these individuals also exhibited an increased accumulation of amyloid proteins in brain regions associated with Alzheimer’s disease.
“Preliminary evidence shows that preclinical Alzheimer’s disease neuropathology is present in young people with youth-onset diabetes.” – Dr Allison Shapiro, author on the study.
The accumulation of toxic amyloid proteins, which form plaques around brain cells and disrupt their function, is a hallmark of Alzheimer’s disease. Although the exact cause of this build-up remains unclear, it initiates many years before any symptoms manifest. This makes early detection and intervention extremely challenging. Subsequent effects of amyloid accumulation include diminished neurotransmitter function and brain shrinkage, notably in memory-related regions.
“These preliminary data suggest the potential for an early-onset Alzheimer’s disease risk trajectory in people diagnosed with diabetes in childhood or adolescence.” – Dr Shapiro.
Additional factors associated with youth-onset diabetes
The researchers express concern about the implications of their findings, especially considering the increasing rates of obesity among youth and the trend of earlier onset diabetes seen in the United States, where the study took place.
“Young people are catching up with adults. We are now seeing more aging-related diseases in young people.” - Dr Shapiro.
Future of youth-onset diabetes and neurodegenerative disease research
The researchers highlight the importance of broadening investigations related to Alzheimer’s disease. This includes exploring the significant role that early-life factors may play in its development. They demonstrate how cognitive testing, typically administered to older adults with diabetes, could also benefit younger individuals.
“The field of diabetes care is beginning to recognise the importance of cognitive testing as a part of clinical follow-up. And it should be something we consider in youth-onset diabetes as well.” - Dr Shapiro.
Looking ahead, the researchers hope to continue testing the same group of individuals as they age. Given the importance of follow-up studies to comprehensively grasp the associated risks and driving factors, this ongoing research could offer valuable clinical insights for doctors managing patients with youth-onset diabetes.
Future research
If you’re interested in learning more about this research, you can access the paper published in Endocrines. If you would like to read more research in this area, please see the Endocrines Special Issue “Advances in Diabetes Care”.